News & Publications
Testing for Candidiasis
September 1, 2013
By Hongxiu Ji, M.D., Ph.D.
Candidiasis is the second most common cause of vulvovaginitis worldwide.1 More commonly referred to as a “yeast infection,” candidiasis occurs when there is overgrowth of yeast. Candida is always present in and on the body in small amounts; however, Candida can multiply when an imbalance occurs, such as when normal acidity of the vagina is altered or when hormonal balance changes. Although these infections can easily be treated, the relapse rate is high. In many instances, this may be due to the potential for misdiagnosis.
The symptoms of candidiasis are similar to those of many other genital infections, so it can be difficult to diagnose a yeast infection by physical examination alone. Sampling vaginal secretions and looking at the sample under a microscope for an abnormal number of Candida organisms is how the diagnosis is usually made. A fungal culture may not always be useful because of the fact that Candida species are already normal inhabitants of the body.
Traditionally, the identification and classification of Candida species were done by time consuming and unreliable methods such as serotyping, colony morphotyping, conventional culture techniques, and morphological and biochemical analysis. In one recent study, the sensitivity of microscopy for diagnosis of Candida vulvovaginitis was only 22%. Physicians diagnosed 54.3% of all Candida infections correctly, but had a false positive diagnosis for 55.6% of all non-infected cases. The use of Amsel criteria or microscopy did not reduce the number of misinterpretations. The study reveals that the misdiagnosis of vaginal complaints can be a problem, which may result in a relapse.2

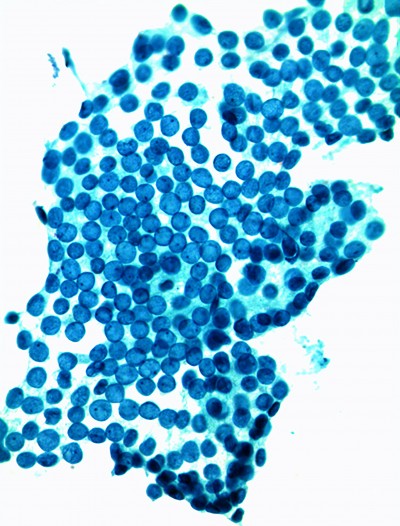
Figure 1
Candida organisms can be seen in Pap collection, usually as filamentous slender structures (see Figure 1), but the Pap test lacks sensitivity in detecting all Candida infections.
Recent improvements in molecular assay technology for identifying Candida species has overcome these previously mentioned limitations during the last couple of years. Polymerase chain reaction (PCR) is a rapid diagnostic assay, which combines many specific species primers in one test, identifying more than one species in a specimen simultaneously.3 The ability to identify the speciation of the infectious process allows clinicians to accurately identify the cause and provide better treatment outcomes. PCR has proven to be a fast and reliable method to identify Candida species.
Incyte Diagnostics chose PCR technology for its molecular infectious disease testing because of its ability to speciate and give providers more information. In addition, the collection procedure has improved. An Incyte Swab is used for a separate specimen collection instead of testing off the Pap collection. This decreases the risk for cross contamination as well as the co-mingling of samples. Also, out-of-vial testing necessitates pre-aliquotting, which can add operational and analytic complexity.
In addition, the detection rate is higher for Candida albicans using the Incyte Swab compared with splitting ThinPrep® or SurePath™ sample types, because swabbing the vaginal walls collects more Candida than sampling the cervix. Testing results have shown:
| Sample Type | Detection Rate | # of Patients | Positive Results |
|---|---|---|---|
| ThinPrep® | 13.65% | 520 | 71 |
| SurePath™ | 11.98% | 192 | 23 |
| Incyte Swab | 18.23% | 1,525 | 278 |
An economic benefit of our PCR testing is ordering only what you want, because you can add other molecular infectious disease tests up to 28 days following collection. This new and innovative PCR technology has been designed to increase diagnostic sensitivity and specificity, while offering the convenience of testing for multiple pathogens from the liquid-based platforms SurePath™ and ThinPrep® you already use. Specimens can be transported at room temperature (no need to refrigerate) and there is a 28-day window for ordering testing of additional pathogens if needed.
Incyte Diagnostics supplies specimen collection materials to our clients. Collection kits contain an Incyte swab collection device, specimen transport medium, requisition form and specimen collection instructions. The turnaround time of the PCR test is two to three business days from sample receipt to test resulting.
Although PCR testing can also be performed out of ThinPrep® or SurePath™ vials that are collected for Pap smears, the use of the Incyte Swab is encouraged. This device is flocked for effective sample collection and subsequent release of the harvest. It contains a fixative to preserve DNA in samples at the time of collection. Other collection devices or transport media may cause pathogen overgrowth and subsequent die-off or allow enzyme excretion during metabolism that may interfere with testing. Once collected, the Incyte swab media is stable for four weeks.
References
1 J. D. Sobel, “Vaginitis,” New England Journal of Medicine, vol. 337, no. 26, pp. 1896–1903, 1997.
2 Andreas Schwiertz*, David Taras, Kerstin Rusch and Volker Rusch. Throwing the dice for the diagnosis of vaginal complaints? Annals of Clinical Microbiology and Antimicrobials Annals of Clinical Microbiology and Antimicrobials 2006,186/1476-0711.
3 G. Luo and T. G. Mitchell, “Rapid identification of pathogenic fungi directly from cultures by using multiplex PCR,” Journal of Clinical Microbiology, vol. 40, no. 8, pp. 2860–2865, 2002.