News & Publications
HNPCC: It’s All Relative
June 1, 2011
By Amy M. Backer, M.D.
In the United States alone, approximately 150,000 people develop colorectal cancer (CRC) each year and it is the third most commonly diagnosed cancer in the world. Adenocarcinoma accounts for 95% of CRC cases but rarer types include lymphoma and squamous cell carcinoma. Most colorectal cancers are preventable through increased surveillance by routine examination and improved lifestyle. Colon cancer is associated with a diet high in fat and beef and low in fiber. If detected early, colon cancer patients have survival rates of 70 to 90%.
The vast majority of colorectal cancers are considered sporadic (isolated instances); however, a small percentage of CRC cases occur in people who have a genetic predisposition. Risk factors for these patients include a family history of colon cancer, especially in a close relative before the age of 55. Individuals found to have hereditary nonpolyposis colorectal cancer (HNPCC), also called Lynch syndrome, have approximately an 80% lifetime risk for colon cancer with a diagnostic mean age of 44 years. Individuals with HNPCC also have an increased risk of other types of cancer.
Women with HNPCC have an 80% lifetime risk of endometrial cancer. HNPCC-associated ovarian cancers have an average diagnosis age of 42 years with 30% of cancers diagnosed under the age of 40 years. It is important to identify HNPCC patients because routine screening of these individuals reduces cancer morbidity and mortality.
Most people with HNPCC inherit the condition from a parent and it develops through changes in their mismatch repair (MMR) genes during DNA replication. This form of genetic destabilization is referred to as the microsatellite instability (MSI) pathway. Microsatellites are repeated sequences of DNA with presumably up to 100,000 microsatellite loci widely distributed throughout the human genome. Each person has microsatellites of a set length, however the length of these sequences is highly variable from person to person. The appearance of abnormally long or short microsatellites in an individual's DNA is called microsatellite instability.
Four markers are tested by Incyte Diagnostics to screen for MSI in colorectal carcinoma. These include mutL homolog 1 (MLH1), mutS homolog 2 (MSH2), mutS homolog 6 (MSH6) and post meiotic segregation increased 2 (PMS2).
| MSH2 | MSH6 | MLH1 | PMS2 | Mutation |
| - | - | + | + | MSH2 |
| + | - | + | + | MSH6 |
| + | + | - | - | MLH1 |
| + | + | + | - | PMS2 |
Generally, MSI detection in two of these markers is considered a positive result or high probability of MSI (MSI-H). Because these enzymes function as complexes, the stability of MSH6 depends on MSH2, and likewise PMS2 depends on MLH1. In cases positive for MMR defect, the IHC pattern helps narrow which germ-line gene to sequence.
MSI analysis is an important tool in pathologic diagnostics because in addition to screening for HNPCC, MSI sporadic tumors have an uncertain response to chemotherapy. Sporadic MSI is associated with approximately 10 to 15% of colorectal, gastric, or endometrial carcinoma and impact clinical prognosis; therefore, the knowledge of a patient's MSI status could help physicians assess prognosis and possibly better guide their therapy.
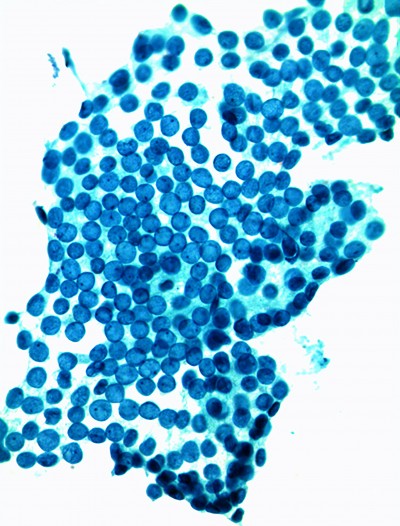
At Incyte Diagnostics, our pathologists are expert in recognizing HNPCC using immunohistochemical (IHC) analysis. Recognizing the presence of specific histological patterns in cancers using IHC testing is an effective standard first-line screening tool. Other forms of testing have emerged recently, but can be three times as expensive with no improvement in sensitivity and specificity. In addition, IHC is the only test currently available that reveals which particular mismatch repair (MMR) gene may be defective, enabling efficient mutation analysis on the target gene.
As technology evolves and more data is available, we may be able to reduce our current panel to include only PMS2 and MSH6. Preliminary data shows that these two antibodies may have the ability to predict mutations on all four MMR genes. Until these findings can be sufficiently validated, our current practice of testing for four markers will remain our preferred choice for first line screening for HNPCC.